
Erika playing at our Ronald McDonald unit after we were discharged from hospital
Chemotherapy:
- Cyclophosphamide – 5 days – 1 hour/day
- Topotecan – 5 days – 30 minutes/day
Discharged – 21st Oct 17
The beginning of her treatment was, of course, scary. We had no idea how she would react to the chemo but we had no choice. It pulls against everything that you feel as a parent. In order to give her a chance at life, we had to make her very sick, on purpose and risk her life to save her life. It sure tugs at the heart strings like I’d never felt before.
Before Erika’s diagnosis, I had no knowledge of what chemotherapy really did to the body. I assumed hair loss and nausea to be the side effects. I was so naïve. Hair loss and nausea were the least of our worries.
Many of the risks are because her immune system would be severely depleted. In fairly simple terms, chemotherapy would knock out the stem cells in her bone marrow which make neutrophils, which are the body’s first line of defence against pathogens. These same stem cells also produce red blood cells, platelets and other immune cells, all of which would become depleted. All previous vaccinations are also wiped out. Not only would she no longer be immune to what she was previously vaccinated for, she would be ill-equipped to fight them with potentially fatal consequences should she catch something. If she were to become ill, her treatment would more than likely be delayed, and that could affect her chances of beating the cancer.
She began preventative medications to reduce some of the risks. Fluconazole, to prevent fungal infections, would be given everyday for the length of her treatment. A broad spectrum antibiotic, Bactrim, would be given twice a day for 3 days a week for the duration of her treatment to help prevent bacterial infection, in particular, lung infections.
The main risk during the first round of chemo was tumour lysis. This is caused by too much rapid cell death which causes an abundance of by-products which the body cannot process fast enough and it can cause lots of complications and is potentially life threatening. We were fortunate that she showed no signs of this.
The chemotherapy was given through the central line. She had IV fluids running 24 hours a day to help protect her organs as well so she was always hooked up to her ‘beep beep’ as she came to call it. After several hours of IV fluids, special chemo nurses came in gowned up and wearing masks and gloves. It was daunting for us all. They needed to take all precautions as exposure to the chemo actually increases their risk of particular cancers themselves. Also once chemo had started, Erika would become cytotoxic and we had to use gloves every time we changed her nappy or dealt with vomit as the same risk applied to anyone tending to Erika and of course this risk applied to her too. The irony of it all was almost amusing if it wasn’t so serious!
We found the nurses to be amazing. After all, why would you work in a children’s oncology ward unless you loved kids and loved helping them. Daily visits by a ‘team’ of doctors were great and as we got to know them, we came to trust them. Dr Tim always made time to call in and see us if things weren’t going so great or if there was any big news but all of his ‘team’ were amazing.

Erika’s ‘Beep Beep’
It was somewhere around this time, when we met Nixon and his family. It was our first contact with another neuroblastoma patient. He was running around in the “bee’ garden at the hospital and was still bright and happy even though he had undergone several rounds of chemo already and had a nasal gastric tube in. Being able to talk to others going through the same thing was very helpful.
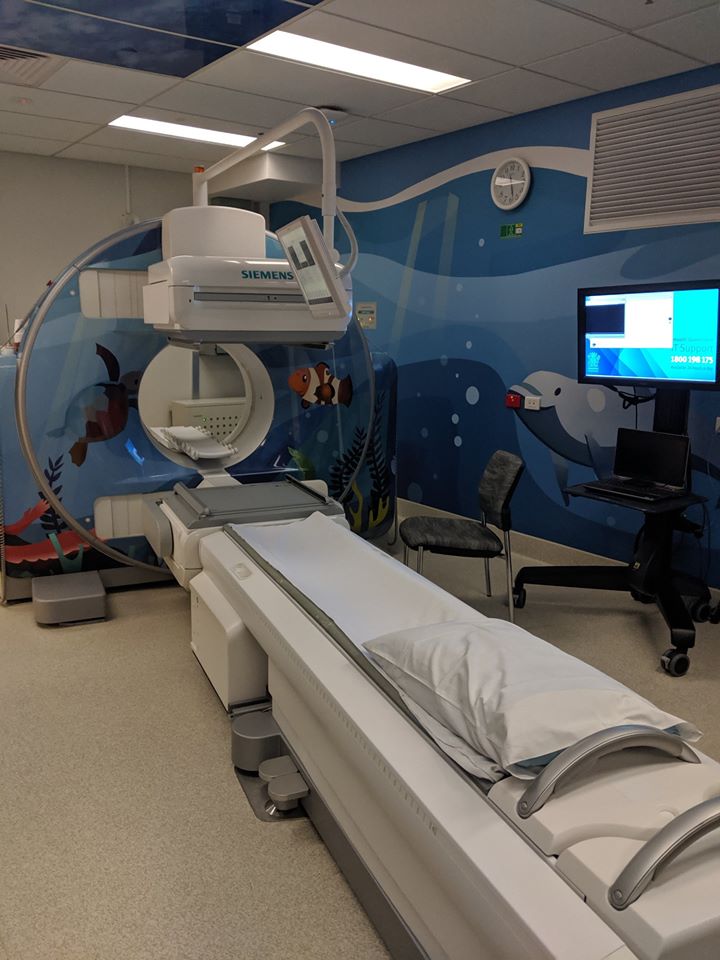
During her first round, Erika had her first of many MIBG scans. First, she had to drink some horrible tasting fluid called lugol iodine, to protect her thyroid from the radiation. We were told it would feel like it was burning the inside of her mouth and throat, and they tried mixing it with some chocolate sauce, but she wasn’t keen on this so we had to hold her down and force her to swallow it. Then, she was given a radioactive chemical through her central line that the neuroblastoma cells suck up and they light up and can be seen on the scan. Then she was swaddled so tight that she couldn’t move, placed on a board and surrounded by large flat detectors that were moved as each section of her body was scanned. She had to stay in it for 60 minutes, and the following day for she had to stay in for 90 minutes. No sedation was given as she did not need to be perfectly still and there would be many times over the next couple of years that she would have to be sedated or have general anesthetics, we needed to use it only when absolutely neccessary. She screamed and struggled the whole time. It broke our hearts. We sang to her, talked to her and tried to get her to watch you tube on a phone. Nothing would comfort her and it was just heartbreaking. During the last phase of the scan, her head was held tight, which freaked her out even more. Fortunately, each time she had an MIGB after this, she got less and less distressed and in the last couple, whilst she still didn’t want to do it, she just watched mummy’s phone and chatted to us. She didn’t like it but she tolerated it.
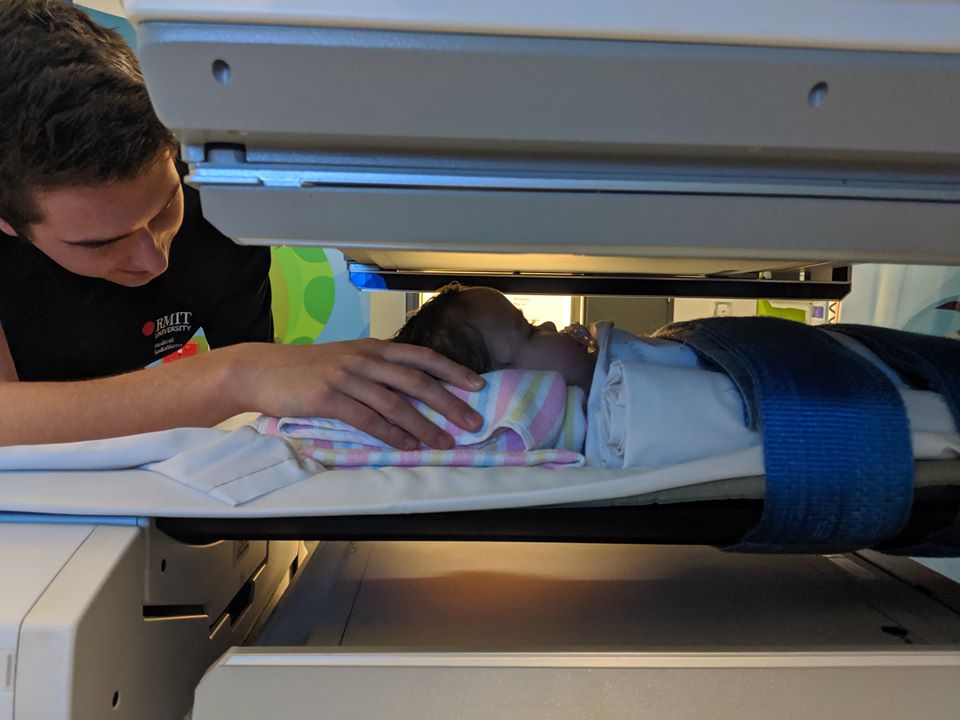
Erika having an MIBG scan later in her treatment. We were far too distressed to even consider photos for the first few
Her first central line dressing change and line care was also done during this time. It was done every week for the duration of her treatment. The fabric dressing around the outside was soaked with remove wipes which helped make it easier to remove but it still stung. Once the dressing was removed, her skin and the external line were disinfected with cold stingy liquid soaked pads, allowed to dry for a minute and then a new dressing was placed back on. The purple bungs on the end of her lines/ lumens were changed and blood was taken for weekly testing. To start with, she also hated this. She screamed and struggled the whole time and it was particularly difficult as hygiene, whilst this was being performed, was critical. If a pathogen were to enter her line, it would be going straight into the bloodstream and be very serious. Lucky for us, she also seemed to get used to this and after a few months she just lay back on Mummy and watched her phone. Again she didn’t like it but seemed to give in to the fact that this was going to be a regular occurrence. We were quite paranoid about her central line and lumens and the potential for them to get caught on something and be ripped out and her pulling on it causing an emergency and risking bleeding to death. We made sure she was always wearing a suit when possible so she couldn’t get to them but it never really became an issue.
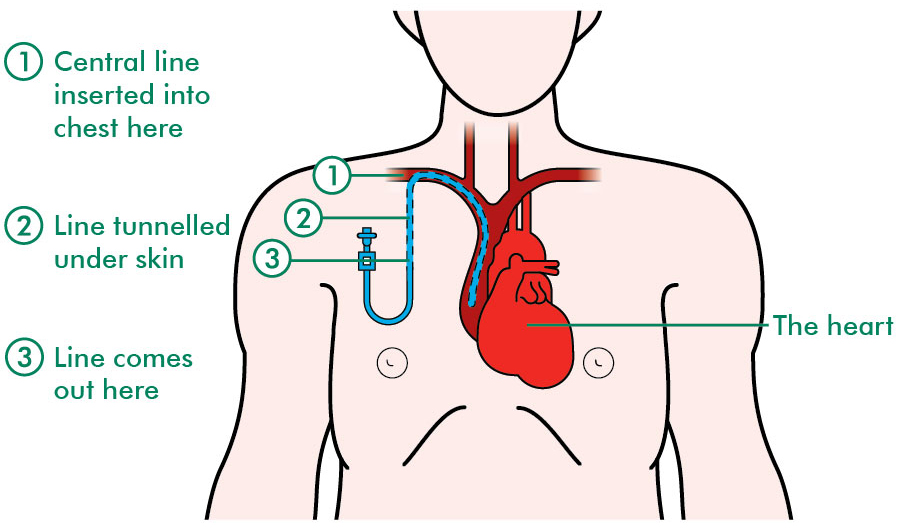

Erika’s central line and dressing and lumens
In between these traumatic but essential events, Erika continued to play happily and thankfully had no idea what all the fuss was about. Once a procedure was over, she would recover very quickly and start playing again. We took solace from this and so intentionally took time to play with her. It kept us busy and less time to ponder over what was happening was good as we couldn’t change anything anyway so we needed to accept it and just get on with it.
We did get some good news this week. The biopsy of her tumour next to her eye came back. There were none of the nasty mutations present so that lifted our heart and increased her chance of survival a bit.
Treatment was risky but it was the best chance she had. No treatment meant no chance at all of growing up. Nicole is a realist and so am I; ignoring something doesn’t change a thing and during this time we had conversations about how we would handle it if Erika didn’t make it. She talked to me of the fear of having anymore children, even if Erika did make it. About how she and Jason promised each other if Erika died they would never leave each other. We also made a promise to ourselves that Erika deserved the very best of us each and every day and that made us able to do just that for most of the time. Also we would deal with what was right in front of us and not focus too far down the track. Nicole amazed and inspired me to support her and Erika as best I could and keep a happy face on when possible.
Once she found her feet, Nicole took it upon herself to be as informed as possible so she researched everything she could online and asked lots of questions to doctors, nurses and other parents in the ward which they gladly answered when possible. She felt comfort in the details and understanding it all from a scientific angle. That doesn’t work for everyone but for her it did.
We were lucky enough to be given a unit not far from the hospital from the Childhood Cancer Support charity and it was only a couple of days after Erika was discharged that we were able to move in there. It was ours for the length of her treatment and it was completely free. No rent, no power bills and anything we needed, we only had to ask. Having this made our ordeal so much more bearable. This is an amazing charity. Erika deserved to have a place to call home so it became known as ‘Erika’s House’.
Apparently the universe thought my feelings needed testing a bit more and we lost Owen’s mum during this round. She was in her 90s and had had a wonderful long life but during her last year, she began to go downhill. Just old age really. She got to meet Erika several times, since she couldn’t remember her each time we went for a visit. She was always so excited when she saw her. Of course, we never told her of Erika’s diagnosis. There was no need. It’s really nice to have photos of them together though. I had to return to Toowoomba for the funeral and it was more difficult than I had anticipated. Sitting in the front row of the chapel, all I could see just a few feet away from me was Nanny’s coffin. I couldn’t stop my mind from seeing a tiny coffin for Erika instead and the reality of losing Erika hit hard and I couldn’t stop the tears. I was fortunate to have plenty of family around me for support. I was probably due for a good cry and felt heaps better afterwards.

Nanny (Ki, Owen’s Mum) with Erika at Yukana in May 2017
Erika got through this round quite well. Her appetite was still quite good, though she enjoyed mostly savoury but not sweet which is quite common in chemo patients. Nicole was still breastfeeding Erika and this was such a good backup and meant the inevitable insertion of a nasal gastric tube was not something we needed to face until BMT time. Once her neutrophils were back up, we were able to go back home to Toowoomba for a few days before the next round began. That was a big surprise as we thought she wouldn’t be able to go home for a long time, and after that, she didn’t.

Visits to her favourite duck park was savoured as we weren’t sure when she would be able to do this again. We kept her away from the general public as much as possible as her immune system had taken a hit. It was however a treasured time and all too soon we had to pack up and drive back to Brisbane to start Round 2.
